The study by Kozlowska et al. (2015), published in the Harvard Review of Psychiatry, provides one of the most comprehensive integrative models of innate threat responses in humans. Drawing upon decades of research in comparative neurobiology and clinical psychiatry, the authors present a multi-phase continuum of autonomically-mediated defense states, termed the defense cascade, which significantly informs our understanding of trauma pathophysiology and clinical practice.
🧩 The Defense Cascade: From Arousal to Collapse
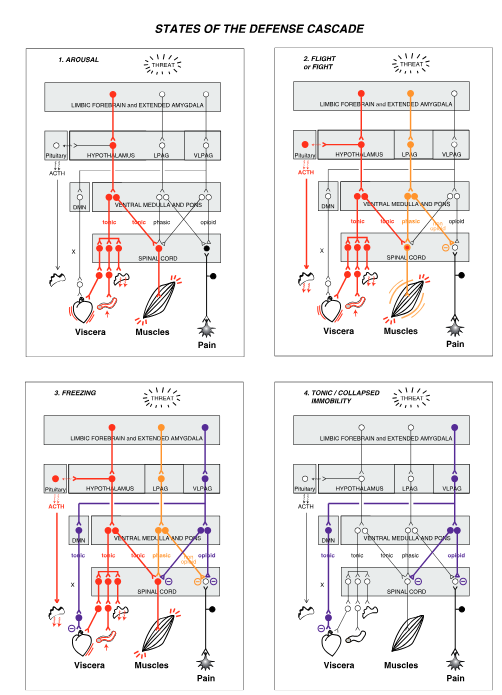
Unlike the oversimplified “fight-or-flight” dichotomy, the defense cascade describes a graduated neurobehavioral sequence:
- Arousal – Sympathetic activation initiated by the hypothalamus prepares the organism for a potential threat, increasing muscle tone, heart rate, and sensory vigilance.
- Flight or Fight – An active defense response mediated by the lateral periaqueductal gray (LPAG). Characterized by motor readiness, non-opioid analgesia, and full somatomotor engagement.
- Freezing – A “pause” in the active defense repertoire, involving co-activation of sympathetic and parasympathetic systems. The ventrolateral PAG (VLPAG) inhibits locomotion while preserving muscle tone, optimizing threat assessment.
- Tonic Immobility – A phylogenetically ancient shutdown response. The subject remains hypertonic but unresponsive, mediated by unmyelinated vagal efferents. Frequently observed in survivors of rape, abuse, or battlefield trauma.
- Collapsed Immobility – Also known as “threat-induced syncope,” this state involves a profound bradycardia-hypotonia-hypoxia triad, often culminating in loss of consciousness. Cerebral hypoperfusion leads to subjective dissociation.
- Quiescent Immobility – A post-threat state enabling physical recovery and parasympathetic rebalancing. It may share pathophysiological features with chronic fatigue and somatoform disorders when prolonged.
Each of these responses is not just behavioral but neuroanatomically distinct, mediated through an interaction of the amygdala, hypothalamus, PAG subregions, medullary centers, and spinal output circuits (see Figures 1 and 2 in the original paper).
🧬 Clinical Relevance and Translational Implications
This cascade has profound relevance for trauma-informed psychotherapeutic protocols. Many patients — particularly those with PTSD, Complex PTSD, dissociative subtypes, or somatization — become “stuck” in one or more of these states, exhibiting persistent neurophysiological patterns that inhibit integration and emotional processing.
Therapeutic strategies informed by this model include:
- Bottom-up interventions targeting autonomic modulation (e.g., vagal tone training, biofeedback, sensorimotor psychotherapy, breathwork).
- Mind-body integration via interoceptive awareness, proprioceptive grounding, and somatic tracking of action patterns or “dispositional representations” (Damasio, 1999).
- Phase-oriented trauma therapies, which scaffold exposure and memory reconsolidation only after foundational skills of arousal regulation are restored.
- Neuromodulatory adjuncts, such as SSRIs, SNRIs, beta-blockers, and alpha-2 agonists (e.g., clonidine), which may restore prefrontal inhibition of limbic hyperreactivity (Etkin & Wager, 2007).
Moreover, advanced imaging has demonstrated that patients in reexperiencing states show hyperactivation of the amygdala and insula, whereas those in dissociative states show prefrontal hypercontrol with amygdala inhibition — further validating the clinical significance of state differentiation (Lanius et al., 2010).
🧠 Conclusion
The defense cascade model constitutes a vital advancement in the neurobiological understanding of trauma. It not only clarifies the complexity of instinctual defense mechanisms but also grounds therapeutic approaches in observable brain-body dynamics. For clinicians, researchers, and tactical trainers working in high-threat environments, such as law enforcement or combat operations, this framework offers essential insights into human responses under duress.
Kozlowska, K., Walker, P., McLean, L., & Carrive, P. (2015). Fear and the defense cascade: Clinical implications and management. Harvard Review of Psychiatry, 23(4), 263–287. https://doi.org/10.1097/HRP.0000000000000065